Prolactin: MOOBS AND MOODS
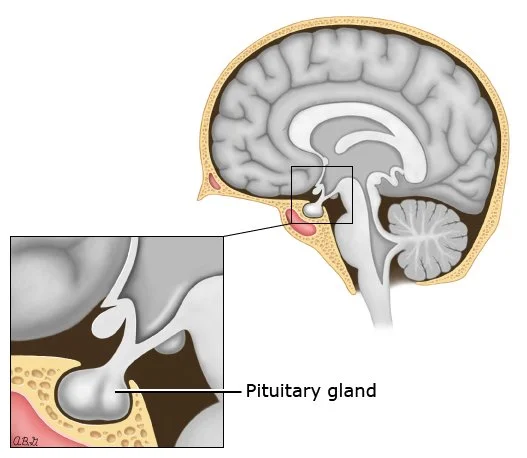
Prolactin is a hormone produced by the pituitary gland that plays a crucial role in the reproductive system of both males and females. In males, prolactin levels are typically low, but there are some situations where they can become elevated.
High prolactin levels in males, also known as hyperprolactinemia, can occur due to various reasons such as a prolactinoma (a non-cancerous tumor in the pituitary gland), medications such as antipsychotics and antidepressants, chronic kidney disease, and hypothyroidism.
Symptoms of high prolactin levels in males may include decreased libido, erectile dysfunction, infertility, gynecomastia (enlargement of breast tissue), and decreased muscle mass. It may also cause reduced body hair growth and osteoporosis in some cases.
If you suspect you have high prolactin levels, it's important to consult a healthcare professional for a proper diagnosis and treatment. The treatment of hyperprolactinemia usually depends on the underlying cause and may include medication, surgery, or lifestyle changes.
Prolactin is a protein that is perhaps best known for its role in milk production. Yet it has influential on >300 known processes in humans and other vertebrates. (1) Prolactin secretes from the pituitary gland as a response to numerous factors such as mating, eating, treatment with oestrogen, ovulation and of course nursing an infant. It plays an essential role in metabolism, pancreatic development and immune regulation. (2, 3, 4)
As discussed, in mammals, prolactin is heavily associated with milk production, but it also acts in a manner similar to cytokines and as a regulator of the immune system, hence my suspicion that the recent increase in high readings amongst data that I have access to is linked to the 2021 increase in inflammatory issues. It acts to in various cell cycle-related functions with growth, differentiation, and anti-apoptotic the main factors. As a growth factor it binds to cytokine-like “receptors”, and influences hematopoiesis and angiogenesis and interestingly is involved in the blood clotting regulation via various pathways.
In both sheep and rats, prolactin has been shown to affect lipid synthesis differentially in mammary and adipose cells. A deficiency in prolactin created using the pharmaceutical drug bromocriptine increased lipogenesis and insulin responsiveness in adipocytes (cells for fat storage) while decreasing them in the mammary gland. (5)
Freeman et al (6) discuss dopamine’s ability to inhibit prolactin, elevated levels of prolactin decrease the levels of the sex hormones, in women oestrogen, and males, testosterone, although this effect varies wildly and how we measure oestrogen.
The “normal” standardised range for men prolactin is 4 to 15 ng/mL (or in the UK 86 to 324 mIU/L may be the range used), my own clinical experience would suggest a range starting as low as 2 through to 18ng/mL (0.02 to 383 mIU/L) and that levels >25ng/mL (532 mIU/L) are considered hyperprolactinemia.
The “optimal” range is suggested to be <7 ng/ml (<149 mIU/L).
Prolactins half-life is suggested to in the range of 15-20 minutes, this blocking synthesis can have fast effects.
What signs make us consider testing for high prolactin?
Reduces libido and fertility (7) Increases stress sensitivity via its action to stimulate the HPA (hypothalamus-pituitary-adrenal) axis (8), in which it increases both CRH and ACTH, that cause higher levels of the stress hormone cortisol. Motivation decreases because prolactin causes a reduction in dopamine synthesis, resulting in symptoms, such as low motivation/drive. (9)
It also increases sensitivity to oestrogen by the mechanism of increasing oestrogen receptors. (10) And because it inhibits steroidogenesis, it lowers testosterone levels. (11) And is correlated with daytime sleepiness, fatigue (12) and increased hair growth in areas such as the back and shoulders. (13)
We may also see, which is interesting given the current epidemic of inflammatory diseases, inflammation and fibrosis of the heart, liver and other organs, autoimmune diseases, such as rheumatoid arthritis (RA), multiple sclerosis (MS) and cardiomyopathy. (14)
One of the major factors many notice is that prolactin inhibits lipolysis while increasing adipogenesis, leading to the enhanced potential for increased adiposity (fat storage) (13) the potential increase in adiponectin tends to increase SHBG, which leads to lower levels of free testosterone (free testosterone is what we need to be able to use), which may for may not be a bad thing depending on your unique situation/results.
What causes prolactin to increase?
The stimulation of prolactin release may be due to many variables, including; serotonin, and as I’ve written previously, approx 95% of serotonin is created in the gastrointestinal tract, and anything that irritates the gut can and will increases serotonin production (fibrous foods etc).
Antipsychotics
Typical
Haloperidol Chlorpromazine, Thioridazine, Thiothixene
Atypical
Risperidone, Amisulpride Molindone, Zotepine
Antidepressants
Tricyclics
Amitriptyline, Desipramine Clomipramine Amoxapine
SSRI
Sertraline, Fluoxetine, Paroxetine
MAO-I
Pargyline, Clorgyline
Other Psychotropics
Buspirone Alprazolam
Prokinetics
Metoclopramide, Domperidone
Antihypertensive
Alpha-methyldopa, Reserpine, Verapamil
Opiates
Morphine
H2 Antagonists
Cimetidine, Ranitidine
Others
Fenfluramine, Physostigmine Chemotherapics (15)
Endogenous
Thyrotropin-releasing hormone (TRH)
Thyroid Stimulating Hormone (TSH)
Angiotensin 2 (16), which is interesting given SARS (Covid-19’s) link to inflammation via the angiotensin system.
Strategies to reduce prolactin
Reduce or avoid the above.
Lower oestrogen, There are several ways to lower oestrogen levels:
Maintain a healthy body weight: Excess fat tissue can convert testosterone to oestrogen, so losing weight (not via starvation) and maintaining a healthy body weight can help reduce oestrogen levels.
Exercise regularly: Regular exercise can help reduce body fat, increase muscle mass, and improve testosterone levels, which can help reduce oestrogen levels.
Eat a healthy diet: Eating a diet rich in fruits, vegetables, and low in processed foods can help maintain healthy hormone levels. (avoid vegetable oils, fasting, low blood sugar, caloric deficits etc).
Avoid alcohol and drugs: Alcohol and drugs can interfere with hormone production and metabolism, so avoiding or reducing their consumption can help reduce oestrogen levels.
Manage stress: Chronic stress can increase cortisol levels, which can lead to decreased testosterone levels and increased oestrogen levels.
Consider medication: In some cases, medication may be necessary to reduce oestrogen levels in men. Your doctor may prescribe medications such as aromatase inhibitors, which block the conversion of testosterone to oestrogen, or selective oestrogen receptor modulators (SERMs), which can help reduce the effects of oestrogen.
It's important to talk to your doctor before making any changes to your diet, exercise routine, or medication regimen, especially if you have any underlying health conditions or are taking other medications.
Aromatase inhibitors are a class of drugs that are commonly used to treat oestrogen-dependent breast cancers. However, they can also be effective in treating pituitary prolactinomas, which are tumours that cause the pituitary gland to produce too much prolactin. Prolactinomas are the most common type of pituitary tumour and can cause a variety of symptoms, including infertility, loss of libido, and irregular menstrual periods in women, as well as erectile dysfunction and decreased sex drive in men. In some cases, these tumours can also cause headaches, vision problems, and even seizures.
Aromatase inhibitors work by blocking the production of oestrogen, which can help reduce the size of the prolactinoma and lower prolactin levels in the blood. This can help alleviate many of the symptoms associated with the condition.
It is important to note that not all prolactinomas will respond to aromatase inhibitors, and treatment options may vary depending on the size and severity of the tumour. Treatment may also involve other medications.
If you have been diagnosed with a pituitary prolactinoma, it is important to work closely with your healthcare provider to determine the best course of treatment for your individual needs.
Aromatase inhibitors are usually more than enough to get prolactin in to range. Anastrozole and cabergoline were sufficient to help treat a prolactin-secreting pituitary adenomas.
“PRL levels decreased in all patients after CAB + ANA (cabergoline + anastrozole) (mean − 70%, range − 44/− 97%), achieving a normalization of PRL levels in one case. Tumor size decreased in all cases (mean − 47%, range − 24.5/− 68%). No severe adverse effects have been reported, a moderate weight gain has been observed in two cases.” (17)
While aspirin is not traditionally thought of as an aromatase inhibitor, there is some evidence that suggests it may have some weak inhibitory effects on the aromatase enzyme. Aromatase is an enzyme that converts androgen hormones to oestrogens. There have been some studies that suggest that aspirin may inhibit aromatase activity, but the evidence is limited and the effect appears to be weak compared to traditional aromatase inhibitors used in cancer treatment. For some this may present a longer term method to reduce oestrogen with over the counter meds.
Major stimulators of oestrogen include stress and sleep deprivation which have been associated with increases in oestrogen levels in men. Stress can lead to an increase in the production of cortisol, a hormone that is produced by the adrenal gland in response to stress. Cortisol has been shown to increase the activity of the enzyme aromatase, which converts testosterone to oestrogen, leading to an increase in oestrogen levels in men.
Sleep deprivation has also been associated with an increase in oestrogen levels in men. Studies have shown that sleep deprivation can disrupt the normal regulation of hormones involved in the reproductive system, including a decrease in testosterone and an increase in oestrogen levels. Additionally, sleep deprivation has been shown to increase the activity of the enzyme aromatase, further contributing to an increase in oestrogen levels.
Overall, both stress and sleep deprivation can contribute to an increase in oestrogen levels in men, although the exact mechanisms by which this occurs are not fully understood. It is important for men to prioritise good sleep habits and stress management to help maintain healthy hormone levels.
Oestrogenic compounds exist at a high level in the modern environment, with plastics bottles, plates, cups, utensils, food wrapping, clothes now common. Processed food often contain emulsifiers, gums, as well as polyunsaturated fats (veg oils).
Optimise thyroid function
Thyrotropin-releasing hormone (TRH) is a hormone produced in the hypothalamus that plays a key role in regulating thyroid function. When released, TRH travels to the pituitary gland and stimulates the release of thyroid-stimulating hormone (TSH), which in turn stimulates the thyroid gland to produce and release the thyroid hormones thyroxine (T4) and triiodothyronine (T3).
Thyrotropin-releasing hormone (TRH) can stimulate the release of prolactin from the anterior pituitary gland. When TRH is released from the hypothalamus, it binds to receptors on the lactotroph cells of the anterior pituitary gland, causing them to release prolactin.
Prolactin is a hormone that stimulates milk production in the mammary glands, but it also has other functions, such as regulating the immune system, metabolism, and reproductive function. The release of prolactin is usually inhibited by dopamine, which is also released from the hypothalamus. However, TRH can override this inhibition and stimulate the release of prolactin.
In addition, high levels of prolactin can also stimulate the release of TRH, creating a feedback loop. This feedback loop can be disrupted in conditions such as hyper-prolactinemia, where there is an excess of prolactin in the blood, leading to a variety of symptoms including menstrual irregularities, infertility, and breast milk production in non-pregnant individuals.
TRH acts on specific receptors in the pituitary gland to increase the production and secretion of TSH. TSH then acts on the thyroid gland to stimulate the uptake of iodine and the synthesis of thyroid hormones. Once synthesised, thyroid hormones are released into the bloodstream, where they act on target tissues throughout the body to regulate metabolism, growth, and development.
Dopamine boost
Dopamine is a neurotransmitter that plays a role in regulating many functions in the brain and body, including the regulation of prolactin secretion. Prolactin is a hormone that is primarily produced by the pituitary gland and is involved in many physiological processes, including milk production in lactating women and the regulation of the reproductive system. Dopamine is produced by neurons in a part of the brain called the hypothalamus, and it can bind to specific receptors on the cells in the pituitary gland that produce prolactin. When dopamine binds to these receptors, it inhibits the production and secretion of prolactin.
This feedback loop between dopamine and prolactin is important for maintaining appropriate levels of prolactin in the body. When dopamine levels are low, for example in individuals with Parkinson's disease who have degeneration of dopamine-producing neurons, prolactin levels can become elevated, leading to a condition called hyper-prolactinemia.
In summary, dopamine reduces prolactin by binding to specific receptors on the cells in the pituitary gland that produce prolactin and inhibiting its production and secretion.
Tonic and phasic dopamine are two different types of dopamine signaling patterns in the brain.
Tonic dopamine refers to the continuous, low-level release of dopamine that is present in the brain at all times. This baseline level of dopamine activity helps to regulate attention, motivation, and other cognitive processes. Tonic dopamine is thought to be involved in maintaining baseline levels of arousal and motivation, and its dysfunction has been implicated in a variety of neuropsychiatric disorders, including depression and addiction.
Phasic dopamine, on the other hand, refers to the rapid, short-term bursts of dopamine that are released in response to specific stimuli or events. These transient spikes in dopamine activity are believed to play a critical role in reinforcement learning, reward processing, and motivation. Phasic dopamine signalling has been extensively studied in the context of addiction, as drugs of abuse can cause a rapid and intense release of dopamine that can lead to addiction and other negative outcomes.
Overall, the interplay between tonic and phasic dopamine signalling is complex and still not yet fully understood. However, it is clear that both forms of dopamine signalling are critical for normal brain function and that their dysfunction can contribute to a variety of neuropsychiatric disorders.
Ideally we want to increase tonic dopamine, the background level of dopamine in the brain, as opposed to the phasic dopamine levels that are released in response to specific stimuli. There are several ways to increase tonic dopamine levels:
Exercise: Regular exercise has been shown to increase dopamine levels in the brain.
Diet: Eating foods rich in tyrosine, an amino acid that is a precursor to dopamine, can help increase dopamine levels. Foods such as almonds, bananas, avocados, and eggs are good sources of tyrosine.
Meditation: Studies have shown that meditation can increase dopamine levels in the brain.
Sleep: Getting enough sleep is important for regulating dopamine levels. Lack of sleep can lead to a decrease in dopamine levels.
Supplements: Certain supplements, such as vitamin D, have been shown to increase dopamine levels in some studies. However, it's important to consult with a healthcare provider before starting any supplement regimen.
Medication: Certain medications, such as antidepressants and stimulants, can increase dopamine levels. However, these should only be taken under the guidance of a healthcare provider. The most popular prescription drugs for hyperprolactinemia are the dopamine agonists, bromocriptine and cabergoline.
Optimise your metabolic function
A study by Davis et al (18), suggests that intracellular calcium plays a role in regulating prolactin mRNA accumulation in GH3 rat pituitary tumour cells. The authors found that increasing intracellular calcium levels with the calcium ionophore ionomycin resulted in an increase in prolactin mRNA levels in these cells. It should be noted that this study was conducted in vitro using rat pituitary tumour cells and may not necessarily reflect the regulation of prolactin secretion in vivo. Additionally, the study focused on the regulation of prolactin mRNA levels, which is a precursor to the synthesis and secretion of prolactin.
While this study provides insight into the regulation of prolactin synthesis, it is important to consider the broader context of prolactin regulation in the body. Prolactin secretion is regulated by a complex network of factors, including hypothalamic hormones, neurotransmitters, and feedback mechanisms. Clinically my experience shows me that in a hypo metabolic state, ATP production is low, and more calcium is taken up into the cell and magnesium is exported. This creates an intracellular excitation that can be seen symptomatically as cramp, right through to tumours (tissue excitation means it can not enter the relaxed state), and we tend to see increased prolactin release.
We want to ensure our bodies are producing optimal amounts of energy (ATP) to help us to maintain an optimal cellular calcium/magnesium balance that also helps to keep prolactin reduced.
Adenosine triphosphate (ATP) is the primary energy source for cellular processes in the body. Increasing ATP production can be beneficial for improving physical performance, increasing metabolism, and enhancing overall energy levels. Here are some ways to increase ATP production:
Exercise: Regular exercise can increase ATP production by increasing the number of mitochondria in the cells. Mitochondria are the powerhouses of the cells, and they produce ATP through a process called oxidative phosphorylation.
Balanced Diet: Eating a balanced diet rich in nutrients like carbohydrates, proteins, and healthy (saturated) fats can provide the building blocks needed for ATP production. The body uses carbohydrates as the primary source of fuel to produce ATP.
Supplementation: Some supplements can help increase ATP production in the body. For example, creatine is a popular supplement that helps increase ATP production in muscle cells.
Sleep: Getting enough sleep is important for ATP production as the body recharges during rest. Lack of sleep can lead to fatigue and decreased energy levels, which can affect ATP production.
DHT
DHT, or dihydrotestosterone, is a hormone that is derived from testosterone through the action of the enzyme 5-alpha reductase. There is limited research on the direct effects of DHT on prolactin levels, but it is generally believed that DHT does not have a significant impact on prolactin secretion. However, it has been shown that it can lower prolactin release at the pituitary gland directly.
Prolactin is primarily regulated by the hypothalamus and pituitary gland in the brain, and is influenced by a number of factors, including stress, sleep, and dopamine levels. Testosterone has been shown to have an inhibitory effect on prolactin secretion by increasing dopamine activity in the brain, which can reduce prolactin release.
However, DHT is a more potent androgen than testosterone, and may have different effects on various physiological processes. Some studies have suggested that DHT may increase prolactin levels in certain circumstances, such as during treatment with certain medications or in individuals with certain medical conditions.
Overall, the relationship between DHT and prolactin is complex and not fully understood. If you have concerns about your prolactin levels, it is best to consult with a healthcare professional who can provide personalised advice based on your individual medical history and circumstances.
Check your testosterone levels
Studies have shown that testosterone can suppress prolactin production in both men and women. One way that testosterone may accomplish this is by inhibiting the release of prolactin-releasing hormone (PRH) from the hypothalamus. Additionally, testosterone can also directly inhibit prolactin synthesis and secretion from the pituitary gland.
Conversely, low testosterone levels may lead to an increase in prolactin production. This is because low testosterone levels can result in decreased negative feedback on the hypothalamus and pituitary gland, leading to an increase in the production and release of prolactin.
Ventilate rather than hyperventilate
There is some evidence to suggest that hyperventilation may increase prolactin levels in some individuals, although the mechanism is not entirely clear. Prolactin is a hormone that plays a role in a variety of physiological processes, including lactation, reproductive function, and stress response.
One study published in the journal Psychosomatic Medicine found that hyperventilation was associated with increased prolactin levels in women with panic disorder, but not in healthy controls. Another study published in the journal Psychiatry Research found that acute hyperventilation was associated with increased prolactin levels in both men and women.
However, it's important to note that these findings are not consistent across all studies, and more research is needed to fully understand the relationship between hyperventilation and prolactin levels. Additionally, hyperventilation can have a range of other effects on the body, including changes in blood pH and carbon dioxide levels, which may also contribute to any observed changes in prolactin levels.
Hyperventilation causes a vast loss of carbon dioxide (CO2), which increases prolactin synthesis. (19) Optimal CO2 level in your blood allows oxygen uptake in to the cells, where as reduced CO2 starves the cells of oxygen, known as the Bohr effect and seen in the hypoxia reported during the c19 pandemic. CO2 acts as a mast cell stabiliser, thus if CO2 depletes, the mast cells release serotonin (and histamine) which in turn increases prolactin.
Nasal breathing can help optimize CO2 levels in the body by allowing for better regulation of CO2 through the respiratory system. When you breathe through your nose, the air you inhale is warmed, moistened, and filtered before it reaches your lungs. The nasal passages also contain structures called turbinates, which help to increase the surface area of the nasal mucosa, allowing for better exchange of oxygen and carbon dioxide.
By breathing through your nose, you increase the amount of time that air spends in your respiratory system, which allows for more efficient gas exchange. This can help to maintain a healthy balance of oxygen and carbon dioxide in the body.
Breathing through the mouth, on the other hand, can lead to excessive loss of carbon dioxide, which can cause a decrease in blood pH and lead to a condition known as respiratory alkalosis. In contrast, nasal breathing can help to maintain healthy CO2 levels and improve overall respiratory function.
Opiate usage
Opiates have been shown to increase prolactin levels in the body, they act on the opioid receptors in the brain, which are also present in the pituitary gland that produces prolactin. When opiates bind to these receptors, it can stimulate the release of prolactin, leading to an increase in its levels in the body. Chronic opiate use can lead to long-term changes in prolactin levels, and high prolactin levels can cause a range of symptoms, including menstrual irregularities, decreased libido, and infertility. Therefore, it is important to monitor prolactin levels in individuals who are taking opiates for extended periods of time.
Opioids, by activating their receptors, stimulate the release of prolactin. Pharmaceutical opioid painkillers such as oxycodone, morphine, fentanyl, tramadol are common causes of high prolactin. Indeed, opioid antagonistic drugs, such as naloxone, effectively lower prolactin. (20)
Reduce inflammation
Inflammation can trigger the release of certain cytokines, which can stimulate the production of prolactin in the pituitary gland. Additionally, chronic inflammation can cause the pituitary gland to become more sensitive to prolactin-releasing factors, leading to an increase in prolactin secretion. (21)
Drugs that increase prolactin
Several drugs can increase prolactin levels in the body, including:
Antipsychotic medications: These drugs, also known as neuroleptics, are used to treat various mental health conditions such as schizophrenia, bipolar disorder, and depression. Examples include risperidone, haloperidol, and chlorpromazine.
Antiemetic medications: These drugs are used to prevent or treat nausea and vomiting, such as metoclopramide and domperidone.
Antidepressant medications: Some antidepressants, particularly the selective serotonin reuptake inhibitors (SSRIs) like fluoxetine and sertraline, can increase prolactin levels.
Hormonal medications: Certain hormonal medications, such as estrogen and oral contraceptives, can increase prolactin levels.
Opioid medications: These pain relievers, such as morphine and codeine, can increase prolactin levels.
It's important to note that while prolactin levels may increase with the use of these medications, the clinical significance and potential side effects of this increase may vary depending on the individual and the specific medication. It's important to consult with a healthcare professional if you have any concerns about your medication regimen or prolactin levels.
SSRIs. Serotonin is a powerful inducer of prolactin release, directly and indirectly by lowering dopamine. (22)
Supplements that can reduce prolactin
Calcium intake and Vitamin D. There is some evidence to suggest that parathyroid hormone (PTH) may have an effect on prolactin levels, but the evidence is limited and the exact relationship between the two hormones is not well understood.
Some studies have suggested that elevated PTH levels may be associated with increased prolactin levels in both men and women, while other studies have found no significant association between the two hormones.
One possible mechanism for this relationship is that PTH may indirectly affect prolactin levels by altering calcium and vitamin D metabolism, as both calcium and vitamin D have been shown to affect prolactin secretion. The parathyroid hormone (PTH) promotes the uptake of calcium. A low calcium diet and low vitamin D levels can increase PTH. When PTH is overactive in can suppress testosterone thus increasing prolactin. (23) It can also suppresses thyroid function that can lead to elevated TRH and prolactin.
Progesterone
Progesterone is a hormone that plays an important role in regulating the menstrual cycle and preparing the body for pregnancy. It has been shown to have an inhibitory effect on prolactin secretion, meaning that it can reduce the amount of prolactin that is released from the pituitary gland.
The exact mechanism by which progesterone reduces prolactin is not fully understood, but it is thought to involve a complex interplay between various hormones and neurotransmitters in the brain.
One possible explanation is that progesterone may act on dopamine receptors in the brain, which are known to inhibit prolactin secretion. Dopamine is a neurotransmitter that plays a key role in regulating the release of prolactin, and progesterone has been shown to increase the activity of dopamine receptors in the brain, thereby reducing the amount of prolactin that is released.
Another possible mechanism involves the regulation of prolactin-releasing hormone (PRH), which is produced by the hypothalamus and stimulates the release of prolactin from the pituitary gland. Progesterone has been shown to reduce the production of PRH, which can help to decrease prolactin levels.
Overall, the exact mechanism by which progesterone reduces prolactin levels is still not fully understood, but it is thought to involve a complex interplay between various hormones and neurotransmitters in the brain.
Progesterone is a hormone that is predominantly found in females, and its role in the regulation of prolactin is mainly studied in females. However, some studies have suggested that progesterone may also have an inhibitory effect on prolactin secretion in males.
Methylene blue
Methylene blue is a medication that has been used for various medical purposes, including as a treatment for methemoglobinemia, a condition in which the blood cannot carry oxygen effectively. While there is some research suggesting that methylene blue may have effects on hormone levels, there is currently limited evidence to suggest that it inhibits prolactin secretion.
One study published in the Journal of Clinical Endocrinology and Metabolism found that methylene blue treatment in healthy men did not significantly affect serum prolactin levels. However, another study published in the same journal found that methylene blue treatment decreased prolactin levels in women with major depressive disorder.
Overall, while there is some limited evidence to suggest that methylene blue may affect prolactin levels, more research is needed to confirm this effect and determine the appropriate dosage and duration of treatment needed to achieve this result. It's always best to consult with a healthcare provider before starting any new medications or making changes to your healthcare regimen.
Vitamin E
There is limited evidence to suggest that vitamin E may have an effect on prolactin levels, but the evidence is mixed and further research is needed to confirm any potential relationship between the two.
One small study published in the Journal of Endocrinological Investigation found that vitamin E supplementation decreased prolactin levels in women with fibrocystic breast disease. However, another study published in the same journal found no significant effect of vitamin E supplementation on prolactin levels in women with infertility.
Aspirin
I use aspirin to reduce the rise in prolactin caused during a stressful sports (or life) activity. (24)
Testosterone (TRT)
There is some evidence to suggest that testosterone replacement therapy (TRT) may help reduce high prolactin levels in men, but the evidence is mixed and more research is needed to fully understand the relationship between the two.
Prolactin is primarily produced in the pituitary gland and plays a role in regulating the immune system, metabolism, and reproductive function. High levels of prolactin in men can cause a variety of symptoms, including reduced libido, erectile dysfunction, and infertility.
Studies have shown that TRT can lower prolactin levels in men with hypogonadism, a condition in which the body doesn't produce enough testosterone. One study published in the Journal of Clinical Endocrinology and Metabolism found that TRT significantly decreased prolactin levels in men with hypogonadism.
However, the relationship between TRT and prolactin levels in men without hypogonadism is less clear. Some studies have suggested that TRT may increase prolactin levels in men with normal testosterone levels, while others have found no significant effect.
Overall, more research is needed to fully understand the relationship between TRT and prolactin levels in men, and to determine the appropriate dosage and duration of treatment needed to achieve any potential therapeutic effects. It's always best to consult with a healthcare provider before starting any new medications or making changes to your healthcare regimen.
References:
Bole-Feysot C, Goffin V, Edery M, Binart N, Kelly PA (1998). Prolactin (PRL) and its receptor: actions, signal transduction pathways and phenotypes observed in PRL receptor knockout mice. Endocrine Reviews. 19(3): 225–68.
Ben-Jonathan N, Hugo ER, Brandebourg TD, LaPensee CR (April 2006). "Focus on prolactin as a metabolic hormone". Trends in Endocrinology and Metabolism. 17(3): 110–116.
Ali M, Mirza L (1 May 2021). Morbid Obesity Due to Prolactinoma and Significant Weight Loss After Dopamine Agonist Treatment. AACE Clinical Case Reports. 7(3): 204–206.
Bates R, Riddle O (November 1935). The preparation of prolactin. Journal of Pharmacology and Experimental Therapeutics. 55(3): 365–371.
Ros M, Lobato MF, García-Ruíz JP, Moreno FJ (March 1990). Integration of lipid metabolism in the mammary gland and adipose tissue by prolactin during lactation. Molecular and Cellular Biochemistry. 93(2): 185–94.
Freeman ME, Kanyicska B, Lerant A, Nagy G (October 2000). Prolactin: structure, function, and regulation of secretion. Physiological Reviews. 80(4): 1523–631.
Levine, S., & Muneyyirci-Delale, O. (2018). Stress-Induced Hyperprolactinemia: Pathophysiology and Clinical Approach. Obstetrics and gynecology international. 2018: 9253083.
Weber, R. F., & Calogero, A. E. (1991). Prolactin stimulates rat hypothalamic corticotropin-releasing hormone and pituitary adrenocorticotropin secretion in vitro. Neuroendocrinology, 54(3), 248–253. https://doi.org/10.1159/000125882
Torner L (2016) Actions of Prolactin in the Brain: From Physiological Adaptations to Stress and Neurogenesis to Psychopathology. Front. Endocrinol. 7:25. doi: 10.3389/fendo.2016.00025
Romero, L., Muñoz, C., López, A., & Vilches, J. (1991). Relación de la prolactina con la hiperplasia nodular y el carcinoma de próstata [Relation of prolactin with nodular hyperplasia and carcinoma of the prostate]. Actas urologicas espanolas, 15(6), 503–509.
Gitay-Goren, H., Lindenbaum, E. S., & Kraiem, Z. (1989). Prolactin inhibits hCG-stimulated steroidogenesis and cAMP accumulation, possibly by increasing phosphodiesterase activity, in rat granulosa cell cultures. Molecular and cellular endocrinology, 61(1), 69–76. https://doi.org/10.1016/0303-7207(89)90190-1
Mogavero,M.P.;Cosentino, F.I.I.; Lanuzza, B.; Tripodi, M.; Lanza, G.; Aricò, D.; DelRosso, L.M.; Pizza, F.; Plazzi, G.; Ferri, R. Increased Serum Prolactin and Excessive Daytime Sleepiness: An Attempt of Proof-of-Concept Study. Brain Sci. 2021,11,1574. https://doi.org/ 10.3390/brainsci11121574
Levine S, Muneyyirci-Delale O. Stress-Induced Hyperprolactinemia: Pathophysiology and Clinical Approach. Obstet Gynecol Int. 2018;2018:9253083. Published 2018 Dec 3. doi:10.1155/2018/9253083
Borba, V, V., Zandman-Goddard, G., & Shoenfeld, Y. (2018). Prolactin and Autoimmunity. Frontiers in Immunology. 9:73.
Torre, D. L., & Falorni, A. (2007). Pharmacological causes of hyperprolactinemia. Therapeutics and clinical risk management, 3(5), 929–951.
Aguilera, G., Hyde, C. L., & Catt, K. J. (1982). Angiotensin II receptors and prolactin release in pituitary lactotrophs. Endocrinology, 111(4), 1045–1050. https://doi.org/10.1210/endo-111-4-1045
Ceccato, F., Lizzul, L., Voltan, G., Barbot, M., & Scaroni, C. (2021). Anastrozole as add-on therapy for cabergoline-resistant prolactin-secreting pituitary adenomas: real-life experience in male patients. Pituitary, 24(6), 914–921. https://doi.org/10.1007/s11102-021-01165-0
Davis, J. R., Vidal, M. E., Wilson, E. M., & Sheppard, M. C. (1988). Calcium dependence of prolactin mRNA accumulation in GH3 rat pituitary tumour cells. Journal of molecular endocrinology, 1(2), 111–116. https://doi.org/10.1677/jme.0.0010111
Odink, J., Wientjes, C. J., Thissen, J. T., van der Beek, E. J., & Kramer, F. M. (1987). Type A behaviour, borderline hyperventilation and psychological, psychosomatic and neuroendocrine responses to mental task load. Biological psychology, 25(2), 107–118. https://doi.org/10.1016/0301-0511(87)90032-9
Mattioli, M., Conte, F., Galeati, G., & Seren, E. (1986). Effect of naloxone on plasma concentrations of prolactin and LH in lactating sows. Journal of reproduction and fertility, 76(1), 167–173. https://doi.org/10.1530/jrf.0.0760167
Tomaszewska-Zaremba, D., Haziak, K., Tomczyk, M., & Herman, A. P. (2018). Inflammation and LPS-Binding Protein Enable the Stimulatory Effect of Endotoxin on Prolactin Secretion in the Ovine Anterior Pituitary: Ex Vivo Study. Mediators of inflammation, 2018, 5427089. https://doi.org/10.1155/2018/5427089
Coker, F., & Taylor, D. (2010). Antidepressant-induced hyperprolactinaemia: incidence, mechanisms and management. CNS drugs, 24(7), 563–574.
Sahovic, V., Sahovic, S., Grosa, E., Avdic, E., Helac-Cvijetic, D., & Kukavica, N. (2012). Correlation between parathormone and sexual hormones in patients on haemodialysis. Medical archives (Sarajevo, Bosnia and Herzegovina), 66(3), 177–180. https://doi.org/10.5455/medarh.2012.66.177-180
Di Luigi, L., Guidetti, L., Romanelli, F., Baldari, C., & Conte, D. (2001). Acetylsalicylic acid inhibits the pituitary response to exercise-related stress in humans. Medicine and science in sports and exercise, 33(12), 2029–2035. https://doi.org/10.1097/00005768-200112000-00009